Why intrauterine insemination, or IUI?
IUI, or intrauterine insemination, is a type of artificial insemination that addresses several causes of infertility.
- Ovulation problems
- Mild male factor infertility
- Unexplained infertility
- Unsuccessful treatment with fertility medications alone
How do I prepare for a cycle?
Before your IUI cycle, you will need to have had a basic fertility workup. This includes lab work, a semen analysis and an HSG to be sure your fallopian tubes are open. Our Dallas-Fort Worth fertility specialists ask you to call the office on Day 1 or 2 of your menstrual cycle. Depending on the type of medication, you may also need an ultrasound. Your doctor will prescribe your medications and tell you when you need to schedule an appointment. Please check your calendar to make sure you and your partner will be in town and available during the treatment process. Our nurse will help you determine when you need to come into the office.
What is the process of intrauterine insemination?
 You can collect the sperm and bring it to our office within 45 minutes. Our lab will then prepare the sperm for artificial insemination and perform a sperm count and motility evaluation.
You can collect the sperm and bring it to our office within 45 minutes. Our lab will then prepare the sperm for artificial insemination and perform a sperm count and motility evaluation.
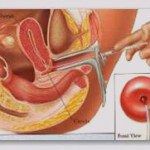
Using a small catheter, the doctor will place the sperm concentrate into the uterus through the cervix. In most cases, IUI is a completely painless process. Sometimes, women may experience cramping, but this is usually very mild and temporary. It is necessary to remain lying down for approximately 10 minutes before you can resume your usual activities.
How do you assess ovulation after treatment?
Progesterone blood testing during the first cycle of treatment can verify ovulation. This occurs approximately seven days following the insemination and a nurse will schedule it. If you have not started your period 14-16 days after the IUI, please do a home pregnancy test and call the nurse with the results.
What is the probability of pregnancy with IUI?
With natural conception in couples without fertility issues, the probability of achieving a pregnancy in any given cycle is approximately 15-20%. In couples undergoing infertility treatment, the chances of pregnancy vary.
IUI increases pregnancy rates by controlling the timing of exposing the eggs to sperm and by increasing the number of sperm that reach the egg. Fertility medications also increase the probability of pregnancy by increasing the number of follicles on the ovary.
In general, the pregnancy rate with Clomid is 6-8% per month and 15-20% with injectable gonadotropins. As a result, gonadotropins with artificial insemination can raise the pregnancy rate to the level experienced by couples without fertility problems. We therefore typically recommend that a couple undergo at least three cycles of treatment before we can evaluate the effectiveness of the therapy.
How many treatment cycles will be needed?
Some couples conceive with only one or two treatment cycles. If no conception occurs after three cycles, your doctor will discuss other options. We understand that there is a physical and emotional toll that fertility treatment takes on patients. As such, we prefer not to continue with a plan that has been unsuccessful after three attempts.
We will review your response and make recommendations about the next steps. Some treatments have a higher probability of success but require more time, effort and cost. We will consider these factors when helping you decide on a new plan.
Does intrauterine insemination have any risks?
The main risk of IUI is the risk of multiple babies in one pregnancy, especially those which are high-order multiple (triplets or more). Our Dallas-Fort Worth fertility specialists try to strike the right balance, but even in the best of hands, high-order multiples can happen. The probability of multiples depends on the type of medications you are taking. For example, the risk of multiples with Clomid is 6-8%. However, with injectable gonadotropins the risk increases to 15-20%.
Multiples, especially high-order multiples, carry risks, including premature delivery. Our goal is to achieve pregnancy with as low a risk as possible to the mother and the newborn child.
Your physician will discuss these risks with you prior to beginning a treatment cycle. However, it is important to note that physicians do not have absolute control over how many eggs are released at the time of ovulation and how many of those eggs are fertilized.
Should I choose IUI or IVF?
For many fertility patients, IUI is the gateway to infertility treatment. Artificial insemination can be the first treatment option if:
- The female partner is under age 35.
- Ovarian reserve is normal for your age.
- Fallopian tubes are patent bilaterally.
IVF is more reasonable if:
- The female partner is over age 35.
- Ovarian reserve is low (high FSH and/or low AMH).
- The cause of your infertility is a severe male factor.
- The history is consistent with tubal disease.
In severe male-factor infertility, artificial insemination may not allow for fertilization because the sperm concentration is too low. Through IVF, sperm can be injected into the eggs in a procedure called intracytoplasmic sperm injection (ICSI). Even when there is no sperm in the ejaculate, in about 80-85% of cases, a urologist can extract sperm from the testicles, which can then be used in ICSI.
Is IUI less invasive than IVF?
There are a lot of fears circulating when it comes to IVF. However, IUI and IVF cycles are very similar. Both require daily self-injections and monitoring with ultrasounds and blood testing. It is true that higher doses of medication are used for IVF, but the main difference is that the IVF cycle requires egg retrieval under intravenous sedation.
Egg retrieval is a minor surgical procedure that involves no incisions. The procedure involves the aspiration of follicles through the vagina with a long needle using ultrasound guidance.
Number of IUIs per cycle
There may be a higher pregnancy rate with more than one insemination per cycle. We suggest starting out with one insemination. If you fail to conceive after two or three cycles, we can go to two inseminations – or – if you prefer, we can start with two inseminations. If you are using a predictor kit, the inseminations occur on the first day of the kit change and the following day. We will provide timing instructions if you are taking fertility medications.
Artificial insemination notes for the Husband
We realize that producing a sperm specimen may be difficult due to the environment. We have collection suites, but if you prefer to collect at home, we offer collection kits at our office. Our team prefers that you provide the sample using masturbation (not interrupted intercourse). If you collect at home, you must deliver the specimen to the lab within 45 minutes and keep it at body temperature.
If the only possible way to collect is through interrupted intercourse, the lab can provide you with a special condom for this purpose. However, it is more difficult for the lab to work with a sample from a condom.
After sample collection, you will be asked to provide several pieces of information to ensure that we correctly identify and process your sample.
First, fill out the provided sticky label with your name and collection information. Attach the label to the sample cup holding the specimen and place it UPRIGHT in the small bag that is provided in the kit. From this point forward, the sample must be maintained between room and body temperature.
Second, bring the sample to our facility. Our lab staff will ask you for a photo ID and for your signature on an identity verification document. You can do this in person, or your partner can deliver the sample for you. If your partner delivers the sample to the lab, she must provide her photo ID and signature.
If you’re ready to explore artificial insemination, contact our Dallas-Fort Worth fertility specialists to schedule an appointment.

